PollerGEN partners reveal link between pollen and increased hospital admissions in London
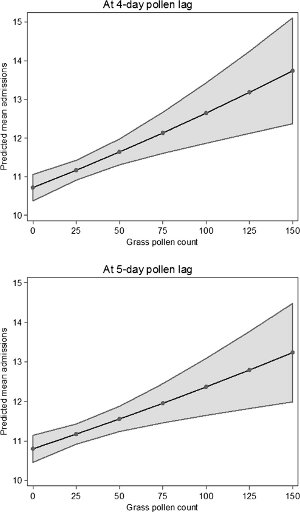 Predicted asthma admissions (95% CI) at representative grass pollen counts at 4-day and 5-day lags Asthma and allergies are some of the most common diseases in many countries globally. UK figures for asthma and hay fever were amongst some of the highest in the world, with one-in-five 6-7-year-olds having asthma and one-in-ten having hay fever. These diseases are termed complex as they have both genetic (over 200 genes associated) and numerous environmental risk factors. Finding out what are the important risk factors is the first step to reducing the burden of this disease in our communities. If the risk factors are modifiable or predictable we may be able to better forewarn patients and their carers of times of high risk, allowing better management of the disease by those who suffer it, and those who plan their healthcare.
Predicted asthma admissions (95% CI) at representative grass pollen counts at 4-day and 5-day lags Asthma and allergies are some of the most common diseases in many countries globally. UK figures for asthma and hay fever were amongst some of the highest in the world, with one-in-five 6-7-year-olds having asthma and one-in-ten having hay fever. These diseases are termed complex as they have both genetic (over 200 genes associated) and numerous environmental risk factors. Finding out what are the important risk factors is the first step to reducing the burden of this disease in our communities. If the risk factors are modifiable or predictable we may be able to better forewarn patients and their carers of times of high risk, allowing better management of the disease by those who suffer it, and those who plan their healthcare.
In this study, PollerGEN partners Nick Osborne and colleagues used existing counts of pollen levels and health episode statistics (cases arriving at emergency departments at hospitals) to examine trends. In London they found daily total grass pollen concentrations from 2005 to 2011 were associated with increased emergency hospital admissions for asthma amongst adults aged 16–64, with a lag of 2 to 5 days between exposure and admission to hospital.
No such effect was seen with a range of tree pollens. While this study confirmed some suspicions researchers had, it also opened up a series of questions including:
- What type of grass is important in this phenomenon?
- Are tree pollens really that different?
- Why such a long lag between breathing in pollen and ending up in hospital?
They are continuing these studies both in the UK and Australia and aim to have some answers to these questions in the near future. Answering these questions will allow better care for the many in our community that suffer asthma and allergies.
(The paper described here is freely available at: https://link.springer.com/article/10.1007%2Fs00484-017-1369-2)
Publication date: 21 June 2017
